Acute compartment syndrome occurs following a rise of pressure in the limb muscle compartment. An episode of
trauma, fractures, contusions and crush injuries account for the majority of cases of compartment syndrome. It can also develop in the setting of strenuous physical activities, patients with hereditary bleeding disorders, therapeutic anticoagulation, microangiopathy due to diabetes, septicemia, animal bites, venous cannulation, intramedullary nailing and as a sequelae of positioning during surgery like lithotomy position during gynaecological procedures and prolonged surgeries like CABG. It needs a high index of suspicion and awareness on the part of clinician to diagnose compartment syndrome, when there is no history of antecedent trauma. Due to medicolegal issues and hesitancy to report unfavourable outcomes, missed compartment syndromes and its catastrophic outcomes are highly under reported. Although there are several studies and reports pertaining to compartment syndrome, there exists several gray areas in the management and often guidelines are unclear.
Timely recognition of compartment syndrome and timely intervention is the single most important factor deciding the outcome. Clinical assessment is still the gold standard. However in equivocal or suspicious scenarios, objective
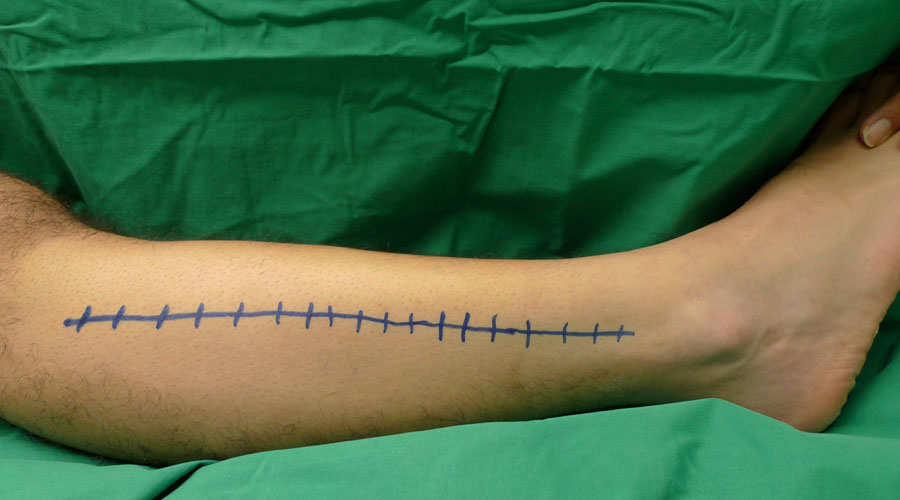
measurement of the compartment pressures can aid in diagnosis. Commercially available portable intracompartmental pressure monitoring systems like stryker quick pressure monitor instrument avoids the need of complex inventory to measure the compartment pressures and are more accurate than techniques like whitesides infusion technique and slit catheter technique [6]. The pressure threshold at which one should decide on fasciotomy was debated at length by various authors. An absolute value of intracompartmental pressure above 30 mm of Hg was suggested by some authors to take as cut off for deciding on fasciotomy. However many investigators later recommended that considering a pressure gradient of 30 to 45 mm Hg (difference between diastolic pressure and intra-compartmental pressure) is more reliable than an absolute value of 30 mm Hg Although the classical dictum in compartment syndrome is to go ahead with fasciotomy when in doubt, one should be aware that the patient reported satisfaction scores regarding fasciotomy wounds and limb function can be categorisedas moderate only. Diability and dissatisfied outcomes of fasciotomy wounds are not uncommon. Wounds can closed in a time span of 5 to 7 days. Vaccum assisted closure devices can be utilised in closure. We alert the clinicians to follow the Ten Commandments when compartment syndrome is under consideration.
The diagnosis of compartment syndrome should be considered based on the clinical findings of ‘wood hard limbs’, tenseness of limbs , pain out of proportion to a perceived cause, pain on passive stretch , increasing need for analgesia , and a compromised neurovascular status.
2. A high index of suspicion is needed to consider the diagnosis of compartment syndrome when there is no history of antecedent trauma.
3. Objective measurement of the compartment pressures can be useful adjunct in establishing the diagnosis. Whenever possible, measure the compartment pressures and document it.
4. A pressure gradient of 30 to 45 mm of Hg (difference between the intra compartmental pressure and diastolic pressure ) is more predictive of compartment syndrome than an absolute value of more than 30 mm of Hg pressure detected in the compartment with pressure monitoring devices.
5. Clinician has to bear in mind that involvement of isolated compartments is not uncommon in compartment syndrome.
6. Fasciotomy wounds are not without problems and quality of life after a fasciotomy are reported as mediocre. Hence clinician should be vigilant and be unbiased taking a balanced view, when establishing the diagnosis.
7. Once diagnosis is established, don’t procrastinate; perform an emergency fasciotomy ensuring adequate release of all affected compartments.
8. Rhabdomyolysis may lead to the accumulation of myoglobin in the kidneys, causing acute renal failure. Adequate hydration should be ensured targeting a urinary output of at least 0.5 mL/kg
9. Delayed intervention can have catastrophic outcomes related to limb and life
10. Proper documentation with history, time of onset, clinical findings and compartment pressures is mandatory in every case.